A survey of 250
Paediatricians reveals a shocking return to old fashioned poverty that will hit
future generations
Nearly one in three
children in the UK – a total of four million – live in poverty.
It’s a statistic that
perhaps many people acknowledge is shocking, but they don’t appreciate its
implications.
Living in poverty can have
all sorts of damaging effects on a child, not least on their health.
Poverty makes children
sick; those living in the most deprived areas have far worse health outcomes than
children from the most affluent.
They are more likely to be
overweight or obese, suffer from asthma, have poorly managed diabetes and
experience mental health problems. Infant mortality is more than twice as high
in the lowest socio-economic groups compared with the highest groups.
Such large numbers can be
a little abstract and it’s only when these are seen as people and personal
stories that the reality hits home.
Comments from more than
250 paediatricians across the UK on the impact of poverty on child health were
gathered as part of a survey by the Royal College of Paediatrics and Child
Health and Child Poverty Action Group (CPAG). It makes sobering reading.
Poor housing
One doctor in London said
that “overcrowded, damp or unsuitable housing among our patients is the rule
rather than the exception” – conditions that can cause respiratory problems
such as asthma and bronchiolitis.
Another said that one of his
patients was a “two-year-old with recurrent seizures, living in a house with no
heating”.
Poor housing is one of the
main reasons for delays in discharging children.
One paediatrician said
they were “unable to discharge a chronically unwell child requiring constant
use of electrical equipment as the house only has one socket”, while another
said: “I have seen a number of babies being unable to be discharged from the
special care babies unit due to parents being homeless.”
Food insecurity
Many respondents said
their patients struggled to afford healthy food.
One doctor observed: “Many
of [our] patients are from low-income families who rely on food banks.”
Another said: “I see
parents in A&E who are limiting their eating to care for their children. Children are worried, scared and upset.”
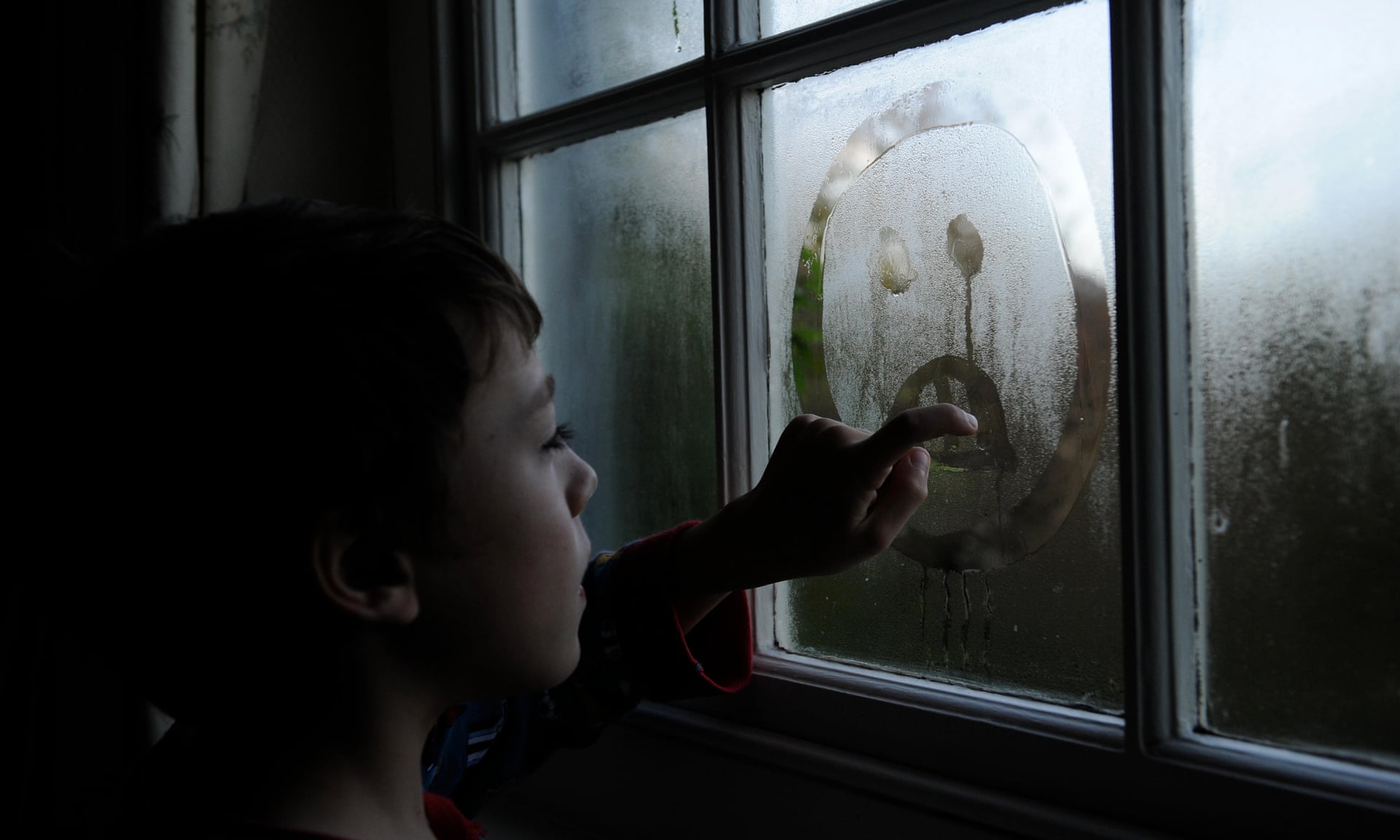
Worry, stress and stigma
Stress and worry caused by
poverty affects not only parents, but children too. One respondent said: “The
biggest impact of poverty on the children and parents I encounter is
insecurity, inferiority and stress. Through biological and psychological
factors these undoubtedly lead to poor health.”
Children who are otherwise
healthy are at risk of becoming unhealthy due to poor nutrition and cold,
cramped housing conditions.
For children who already
have health problems, poverty exacerbates the difficulties.
One doctor said, “For
sickle cell patients, cold homes can precipitate painful crises and admission
to hospital” while another commented that “overcrowding makes looking after
children with learning difficulties or autism next to impossible”.
One of the things that
shocked me about the stories from the report is that we are seeing the return
of what one might think of as old-fashioned poverty relating to crowding and
nutrition for our children.
Political will
If poverty levels were
reduced, the impact on child health – and therefore the future health of the
nation - would be radical.
Whatever political party
holds the reins of power post 8 June, tackling poverty must be a priority.
We need the next
government to focus on the creation and maintenance of wealth for all parts of
society, with a focus on our children.
Policies such as the
restoration of binding national targets to reduce child poverty, backed by a
national child poverty strategy and the adoption of a “child health in all
policies” approach to decision making and policy development, with the Treasury
disclosing information about the impact of the chancellor’s annual budget
statement on child poverty and inequality, could make a difference.
There should also be an
immediate reversal of public health cuts to ensure universal early years
services, including health visiting and school nursing, are prioritised and
supported financially, with additional targeted help for children and families
experiencing poverty.
The health of children is
a measure of the future health of our society. As one of the doctors who
responded to the survey said: “We cannot expect to have a healthy future for
the UK if we leave our children behind.”
Source: The Guardian